Enhancing Urea Cycle Disorder Research with the Biochrom 30+ Amino Acid Analyzer
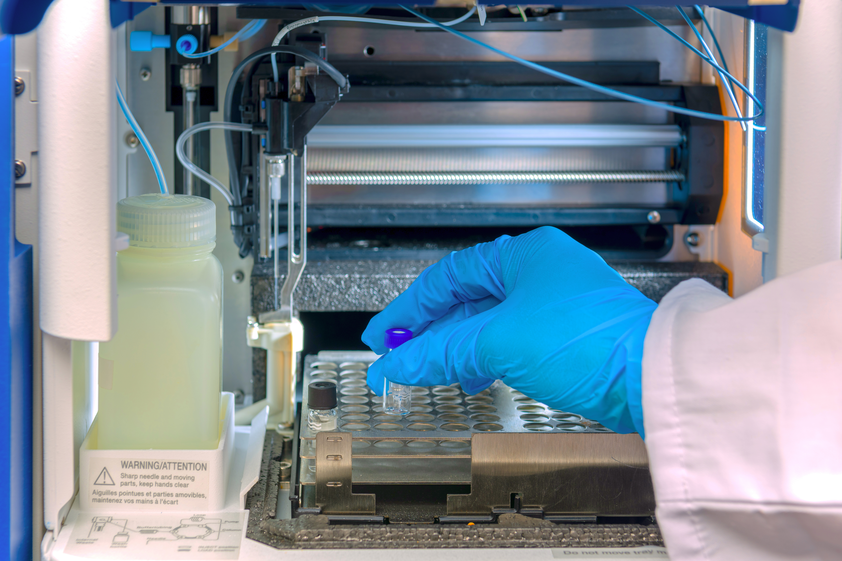
A recent study from Great Ormond Street Hospital suggests that commonly prescribed nitrogen scavengers for Urea Cycle Disorders (UCD) may contribute to Branch Chain Amino Acid (BCAA) depletion, highlighting the need for a balanced approach that optimizes protein intake and considers alternative treatments.
In patients with Urea Cycle Disorders (UCD), the liver lacks an essential enzyme required to convert nitrogen into urea. This deficiency leads to a toxic accumulation of ammonia in the bloodstream, known as hyperammonemia, which, if untreated, can result in brain damage, coma, and death.
UCD encompasses multiple disorders, each involving a deficiency or absence of different enzymes, with varying levels of severity. Established treatments focus on controlling ammonia levels through dialysis, followed by maintenance with nitrogen scavenger medications and a carefully regulated dietary protein intake.
Branch Chain Amino Acids (BCAAs) – leucine, isoleucine and valine – are essential amino acids for muscle growth and metabolic stability, comprising 30-40% of dietary protein intake. A recent study from Great Ormond Street Hospital using the Biochrom Bio 30+ Amino Acid Analyzer found that patients receiving commonly prescribed nitrogen scavengers such as sodium benzoate (NaBz) or sodium phenylbutyrate (NaPBA), were more likely to exhibit low BCAA levels. This suggests that while scavengers help control ammonia, they may also contribute to BCAA depletion.
The researchers observed an inverse correlation between protein intake and plasma BCAA levels, particularly in patients using NaBz. To mitigate this, clinicians should optimize the biological value of dietary protein and, when necessary, introduce essential amino acid (EAA) supplements to prevent deficiencies. The study also highlights that hyperammonemia itself may contribute to BCAA depletion. Effective ammonia control—not only through scavengers but also by ensuring adequate yet safe protein intake—could help maintain BCAA balance.
At Great Ormond Street Hospital, patients transitioned from NaBz to glycerol phenylbutyrate (GPB) exhibited improved ammonia control without further BCAA depletion, suggesting that GPB may be a more favorable option for preserving metabolic balance in UCD patients.
The study’s authors speculate that low BCAA levels in UCD patients — previously attributed to high plasma ammonia and nitro scavenger use — may actually serve as proxy indicators of disease severity. This challenges the current understanding of the cause-and-effect UCDs. If more severe cases are inherently prone to BCAA depletion, these individuals may require higher scavenger doses to control ammonia, which, in turn, could allow for increased dietary protein and supplementation to improve outcomes.
This research underscores the importance of a comprehensive approach to UCD management—one that not only controls ammonia levels but also preserves essential amino acids to support better patient health and development.